Update on iatrogenic botulism cases in Europe
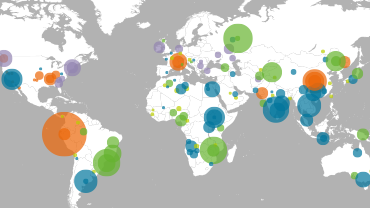
Since late February 2023 and up until 30 March 2023, 87 cases of botulism linked to intragastric injection of the botulinum neurotoxin (BoNT) have been reported in Germany (30), Austria (1), France (1), Switzerland (2), and Türkiye (53). This is an increase of 18 cases in Germany, and one new case each in France and Switzerland, since the last ECDC update on 10 March 2023.
The information currently available indicates that all the cases had medical interventions aimed at helping them lose weight. These were performed between 3 February and 1 March 2023 in Türkiye. The cases are reported to have received intragastric botulinum neurotoxin (BoNT) injections for the treatment of obesity at two private hospitals: one in Istanbul and another in Izmir. Germany has reported that for the German patients, the injected doses ranged between 1 000 and 2 500 units of BoNT.
The symptoms ranged from mild to severe, and several cases have been hospitalised. Among those hospitalised, a number are reported to have been admitted to intensive care units (ICU) and received treatment with botulinum anti-toxin.
Individuals who have travelled to Istanbul and Izmir for intragastric BoNT treatment between 3 February and 1 March 2023, are encouraged to seek medical advice from their healthcare providers, particularly if they experience symptoms such as weakness, difficulty in breathing and/or swallowing. ECDC strongly encourages EU/EEA citizens to avoid intragastric treatments with BoNT for obesity in Türkiye, as this is currently associated with a significant risk of developing botulism.
Investigations carried out by Turkish authorities revealed that licensed BoNT products were administered off-label for the treatment of obesity by intragastric injections. Consequently, the relevant departments of both the hospitals have had their activities suspended, and investigations have been launched against the parties involved.
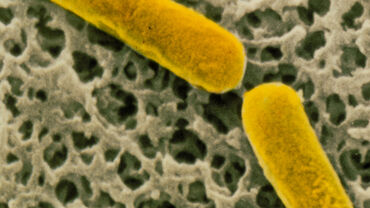
Botulism is a serious neuroparalytic illness caused by BoNTs mainly produced by the bacterium Clostridium botulinum. The disease naturally occurs in four different forms:
- food-borne botulism, caused by eating food containing BoNTs;
- intestinal botulism, when botulinum spores germinate within the intestine of adult persons;
- infant botulism, when botulinum spores germinate within the intestine of babies under one year of age;
- wound botulism, when a wound gets infected by botulinum spores.
There are two other forms of botulism which do not occur naturally: inhalation botulism and iatrogenic botulism, of which the latter may occur as an adverse event following the administration of BoNTs for therapeutic or cosmetic reasons.
While it is considered rare, individuals receiving BoNT injections for cosmetic purposes (for example, for facial wrinkle lines) or therapeutic treatments (for example, management of muscle spasticity), may develop botulism if they are injected with an excessive dose of BoNTs.
Symptoms of iatrogenic botulism include weakness and fatigue. Toxicities following cosmetic treatment can include blurred vision, drooping eyelids, difficulty in swallowing, and dry mouth. Toxicities following therapeutic treatment can include difficulty in breathing, indicating the administration of an overdose.
The symptoms of botulism can be very severe, and require intensive-care treatment as well as the administration of botulinum anti-toxin. Even when such treatments are available, complete recovery usually takes weeks to months. Limited information is available onmortality rates in botulism cases caused by medical interventions. For food-borne botulism, 5–10% of the cases are fatal.