Clostridioides (Clostridium) difficile infections - Annual Epidemiological Report for 2016–2017
In 2016–2017, 1 559 hospital surveillance periods were reported, corresponding to >18.3 million patient admissions and >109 million patient-days.
Executive summary
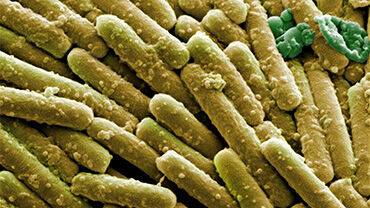
On 1 January 2016, ECDC started coordinating the surveillance of Clostridioides (Clostridium) difficile infection (CDI) in acute care hospitals in EU/EEA countries. ECDC’s surveillance protocol provides a standardised tool for hospitals to measure and monitor CDI incidence rates, with three surveillance options, i.e. a ‘minimal’, a ‘light’ and an ‘enhanced’ option, the latter linking case-based epidemiological and microbiological data [1]. This report includes CDI surveillance data from 2016–2017.
In 2016–2017, 24 EU/EEA countries/administrations (UK devolved administrations are counted separately) reported CDI data to ECDC, of which 23 countries had data suitable for analysis. These countries/administrations reported 1 559 hospital surveillance periods corresponding to >18.3 million patient admissions and >109 million patient-days.
For 2017, CDI data were contributed by >21% acute care hospitals in the participating countries/administrations, and >10% of all acute care hospitals in the EU/EEA. Ten participating countries/administrations (Belgium, Hungary, Iceland, Ireland, Lithuania, the Netherlands, Malta, UK-England, UK-Scotland and UK-Wales) had 85%–100% national coverage in 2016 or 2017, in terms of the number of participating acute-care hospitals or acute care hospital beds. However, comparisons between the two years should only be made cautiously, as only 14 (61%) countries/administrations contributed data for both 2016 and 2017.
Overall in 2016–2017, 72.0% of the CDI cases with case-based data were above 64 years old and the majority (56.4%) were female. More than half (n=3 446/5 863; 58.8%) of the CDI cases had had contact with healthcare in the three months before the current healthcare admission, of which the vast majority (n=2 804/3 446; 81.4%) had had contact with a hospital. Fewer were reported to have had contact with a long-term care facility (LTCF) (n=431; 12.5%).
Information on the outcome of CDI was available for 11 568/26 825 (43.1%) cases, of which 2 029(17.5%) cases died, from any cause. Death was reported as ‘possibly’ or ‘definitely’ related to CDI for480 (4.1%) of 11 568 CDI cases with known outcome. Considering this rate, and that there were an estimated 189 526 healthcare-associated (HA) CDI cases (cumulative 95% confidence interval (95%CI): 105 154–340 978) in EU/EEA countries/administrations annually in 2016–2017 [2], this suggests that there were 7 864 fatal HA CDI cases (95% CI: 4 363–14 148) annually in the EU/EEA for whom CDI had contributed to their fatal outcome.
At the case-level ECDC CDI incidence surveillance data for 2016–2017, there were 1 792/12 097(14.8%) cases that were reported to have a ‘complicated course of infection’, according to the ECDC and European Society of Clinical Microbiology and Infectious Diseases (ESCMID) definition, i.e. admission due to community-onset CDI; admission to an intensive care unit (ICU); surgery(colectomy) for toxic megacolon, perforation or refractory colitis; or death.
In 2016–2017, the crude incidence density of CDI was 3.48 cases per 10 000 patient-days. This was higher in tertiary care hospitals (3.87 cases per 10 000 patient-days) than in secondary or primary care hospitals(3.46 and 2.28 cases per 10 000 patient-days, respectively). Tertiary hospitals were commonly large, university-affiliated, teaching hospitals while primary hospitals were commonly general hospitals with no teaching activity and few specialities and laboratory services. The crude incidence density was the lowest in the heterogeneous group of ‘specialised’ hospitals (2.24 cases per 10 000 patient-days).
In 2016–2017, 23 052/37 857 (60.9%) cases were HA CDI. The vast majority of HA CDI cases had their origin in the current hospital (n=13 576/16 101; 84.3%), with far fewer cases being associated with another hospital(n=815; 5.1%), an LTCF (n=514; 3.2%) or ‘other healthcare’ (n=228; 1.4%). Tertiary care hospitals had the highest mean hospital-level HA CDI incidence (2.75 cases per 10 000 patient-days), followed by secondary care, specialised and primary care hospitals (2.21, 1.63 and 1.46 cases/10 000 patient-days, respectively).
In 2016–2017, 2 439/37 857 (6.4%) CDI cases were reported to be recurrent. Amongst the recurrent CDI cases, death during the current hospitalisation was reported as ‘possibly’ or ‘definitely’ related to CDI for 50/160 (31.3%) fatal recurrent CDI cases, which was 67% more than for fatal non-recurrent CDI cases (224/1 273; 17.6%)(p=0.001). Additionally, recurrent cases were almost twice as likely to have a complicated course of infection(290/1 162; 25.0%) than non-recurrent cases (1 140/8 079; 14.1%) (p<0.0001).
In 2016–2017, 12 366/37 857 (32.7%) CDI cases were community-associated (CA CDI), or CDI of unknown association (UA CDI). The proportion of CA CDI cases reported to have had prior contact with an LTCF was 13.6% (107/787), which was more than twice the proportion reported for all CDI cases (n=324/5 076; 6.4%).
In 2016–2017, while the mean hospital rate of CDI testing was 96.1 stool tests per 10 000 patient-days, the median rate was 38.6 stool tests per 10 000 patient-days, as many hospitals tested relatively infrequently.
ESCMID-recommended diagnostic algorithms were used during 902/1 175 (76.8%) hospital surveillance periods [3,4].
10 countries/administrations reported PCR ribotype (RT) data for their CDI cases, of which three countries/administrations (Belgium, the Netherlands and UK-Wales) reported 3 889/4 832 (80.5%) of these cases. Therefore, the RT data are not likely to be representative of the EU/EEA as a whole.
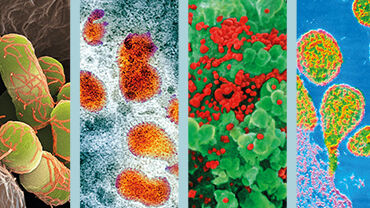
14 of the 20 most commonly reported RTs were Clade 1, including the most common RT, RT014/020(814/4 865 reports; 16.8%). RT014/020 was the most frequent, or the second most frequently reported RT in seven countries/administrations. RT078 (Clade 5), which is commonly detected in one-health investigations, particularly involving pigs, was reported relatively frequently by Belgium, Czechia, Ireland and the Netherlands (7–11% cases).
RT027, which is known for its hypervirulence [5,6], was the third most frequently reported RT in2016–2017. It was notably prevalent in the cases reported by Hungary (67.6%), Poland (63.0%) and Slovenia (44.4%), compared to cases from all other countries/administrations (2.5%). Four countries(Czechia, Hungary, Poland and Slovakia) reported 78/86 (90.7%) of RT027-like RTs (C. difficile Clade2, multi-locus sequence type (MLST) 1, e.g. RT176, RT036/198, RT016 and RT181). RT181 strains were also identified in cases reported by Greece.
The reports of the detection of metronidazole resistance by E-test are of concern, as metronidazole was among the first-line treatment options recommended by ESCMID and the Infectious Diseases Society of America (IDSA) for certain subsets of CDI cases [7,8]. The 2021 update of the ESCMID guidelines no longer recommends metronidazole for treatment of CDI when fidaxomicin or vancomycin are available [9].
In 2016–2017, all but one of the metronidazole-resistant isolates were RT027 (20/26; 76.9%) or theRT027-like strain, RT036/198 (5/26; 19.2%). EU/EEA countries should consider confirming metronidazole resistance and vancomycin resistance of C. difficile isolates by agar dilution methods, performed by a reference laboratory, and conducting additional investigations to elucidate the transmission mechanisms.
ECDC recommends continual incidence surveillance of CDI for a period of 12 months. If not feasible, ECDC recommends a minimum surveillance period of three months. The update of the ECDC surveillance protocol for 2020 also contains structure and process indicators of infection prevention and control, including the optional collection of antimicrobial consumption data in participating hospitals.