About ERLI-Net
The main objectives of ERLI-Net are to carry out virological surveillance of human influenza and to ensure that data are shared through the European Influenza Surveillance Network (EISN) reporting mechanisms in a timely manner.
ERLI-Net comprises nominated expert representatives from laboratories in all EU Member States and two EEA countries (Norway and Iceland).
ERLI-Net has its roots in the Community Network of Reference Laboratories for Human Influenza in Europe (CNRL) which was established in 2003 to formalize the network of national influenza reference laboratories participating in the European Influenza Surveillance Scheme (EISS). From 1 September 2008, the coordination of influenza surveillance activities was transferred to the European Centre for Disease Prevention and Control (ECDC). The network was renamed the European Influenza Surveillance Network (EISN). In June 2013, CNRL was renamed The European Reference Laboratory Network for Human Influenza (ERLI-Net).
ECDC coordinates all activities related to ERLI-Net. This includes those activities delivered by external contractors such as the central characterization of influenza viruses, external quality assessment (EQA), wet lab and online training for network members, and monitoring of influenza-related mortality in Europe.
Mechanisms of working
The ERLI-Net coordination group aims to capitalise on the expertise within network laboratories by continuing to use dedicated virology task groups to complete specific activities. This model of working has facilitated discussion and enhanced working relationships within the network by sharing best practices and harmonising technical approaches. A wider meeting of all EISN virologists takes place once a year.
Collaboration with WHO
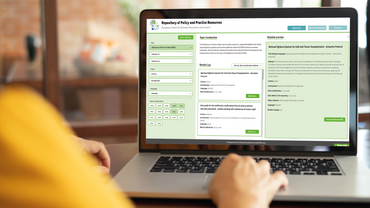
Most ERLI-Net laboratories are also WHO-recognised National Influenza Centres (NIC). They are supported by the WHO Collaborating Centre for Reference and Research on Influenza, London, UK (WHO CC). The NICs participate in the Global Influenza Surveillance and Response System (GISRS). The EU/EEA Member State laboratories that are members of ERLI-Net report their surveillance data to The European Surveillance System (TESSy) database hosted by ECDC. Data from TESSy are transferred to the to the Flu News Europe, the Joint ECDC-WHO/Europe weekly influenza update. All European NICs have agreed to the Pandemic Influenza Preparedness (PIP) Framework and to its influenza virus traceability mechanism (IVTM), as have their national governments through the World Health Assembly in May 2011 (Motion 64.5).
Key tasks of the network
Since its establishment, ERLI-Net has been working to improve EU national influenza reference laboratory capabilities and capacity. In order to ensure the reporting of accurate virological data to EISN, laboratories participating in ERLI-Net must be able to perform a range of key virological technical tasks.
Key tasks include:
- Direct detection of influenza virus types A and B using molecular methodology;
- Influenza virus culture, essential to retain for vaccine strain formulation;
- Determination of type and subtype of seasonal influenza using specific nucleic acid amplifications;
- Ability to detect viruses with pandemic potential (H5 or other avian influenza virus strains);
- Antigenic characterisation of seasonal influenza strains (ideally supported by genetic characterisation);
- Storage of clinical specimens and virus isolates;
- Shipment of virus isolates and/or clinical specimens to the WHO CC in London;
- Participation in external quality assurance (EQA) exercises;
- Electronic reporting of data nationally and internationally.
Within ERLI-Net, it is recognised that laboratory capability varies. Laboratories with appropriate capabilities and capacity should also perform additional complementary tasks. Laboratories without capability or capacity should refer samples for testing to the WHO-CC or another ERLI-Net laboratory under a collaborative agreement.
Additional complimentary tasks include:
- Genetic characterisation by sequencing HA and NA of influenza virus types A and B;
- Subtyping of zoonotic influenza viruses;
- Antiviral susceptibility monitoring.
Direct detection of influenza virus A and B
Laboratories should be able to detect the presence of influenza virus in a clinical specimen using genetic detection (RT-PCR) and, for example, by antigenic assays (immunofluorescence, ELISA or commercial kits). Detection, typing and/or subtyping of influenza virus can be done simultaneously using type and/or subtype-specific molecular methodology.
Culture of influenza virus
Laboratories must be able to grow influenza virus from clinical specimens for detection, typing and subtyping. Growth on tissue culture cell lines is an essential requirement. Growth of influenza virus in embryonated eggs (required for the bi-annual selection of vaccine candidate viruses) is not a key task. Growth of virus can be detected using the genetic and antigenic techniques described above, and by haemagglutinating activity of the tissue culture supernatant or egg allantoic fluid. Assays for viral neuraminidase activity can also be used.
Determination of type and subtype of seasonal influenza and H5 viruses
ERLI-Net members should be capable of detecting, typing and subtyping the following viruses as a minimal requirement:
- Influenza virus A/H1
- Influenza virus A/H3
- Influenza virus A/H5 or other avian influenza virus strains
- Influenza virus B
Laboratories should be able to type the haemagglutinin (HA). Typing and subtyping can be done genetically (type- and subtype-specific RT-PCR) and antigenically (e.g. by the haemagglutination inhibition assay and/or virus neutralisation assay). Any viruses that cannot be subtyped (unsubtypeable) should immediately be referred to a reference laboratory. Influenza A/H5 or other avian influenza viruses must be sent immediately to a WHO-CC or WHO H5 Reference Laboratory for confirmation.
Antigenic characterisation of influenza virus
Antigenic characterisation of the haemagglutinin is important for determining how well-matched currently circulating viruses are to the recommended vaccine virus, and for the selection of vaccine candidate viruses. Laboratories should be able to perform antigenic characterisation on at least a selection of cultured virus isolates. Current human vaccine viruses and a limited supply of homologous post-infection ferret antisera are available from the WHO-CC, London. Any unsubtypeable viruses should be referred to a reference laboratory immediately.
Antiviral susceptibility testing
Some European laboratories monitor influenza virus susceptibility to neuraminidase inhibitors (NAI). Phenotypic screening of virus isolates by MUNANA or NA-STAR assays is the ‘gold standard’ allowing determination of resistance phenotype and monitoring of trends in antiviral susceptibility. Linked with gene sequencing, results can be related to known resistance-conferring mutations and identification of resistance conferred by novel mutations. Genotypic screening for well-characterised substitutions such as H275Y in N1 NA which confers resistance to the NAI Oseltamivir can be performed by SNP (single nucleotide polymorphism) detection PCR or cycle- or pyro-sequencing.
Antiviral susceptibility testing is a complementary task that should either be performed by the laboratory itself, or by referral of a selection of viruses to a collaborating laboratory. Data should be reported in a timely manner to the European Surveillance System (TESSy) database. These data are analysed and interpreted by members of the ERLI-Net Coordination Group and presented in the Flu News Europe, the Joint ECDC-WHO/Europe weekly influenza update.