Interim public health considerations for COVID-19 vaccination roll-out during 2023
This document offers an overview of the available scientific evidence and epidemiological situation and provides public health considerations to support discussions and decisions on the planning and implementation of COVID-19 vaccination campaigns for 2023.
Executive summary
Severe COVID-19 continues to disproportionately affect older adults and individuals with underlying comorbidities. Each time there has been a new wave of infection, EU/EEA countries’ surveillance data from 2022 onwards indicate the largest increases in hospital, intensive care unit (ICU) admissions and deaths in the age groups 65−79 and 80 years and older. However, the height of the peaks for these indicators is lower than in the pre-Omicron period. Similarly, length of hospital stay increases with age, and is longest in individuals aged 65 years and above and especially those aged 80 years and above.
At this stage of the pandemic, the main objectives of COVID-19 vaccination campaigns continue to be reducing COVID-19 hospitalisations, severe disease and deaths, and protecting healthcare systems.
In 2022, all EU/EEA countries recommended the administration of COVID-19 booster doses, mostly for older population groups such as those aged 60 years and above, individuals with underlying medical conditions and other selected groups. In those aged 60 years and above, uptake of the primary series and first booster has levelled off in all countries over the last year (>90%; > 40%, respectively). The uptake of the second booster shows a less evident pattern and more heterogeneity across countries. In general, every subsequent booster dose added to vaccination campaigns shows lower uptake.
Despite only a fraction of infections being detected, reported COVID-19 case rates fluctuate around levels comparable to those reported during late 2020 and 2021 – prior to Omicron circulation and when widespread free population testing was available. This suggests high levels of ongoing SARS-CoV-2 transmission in the EU/EEA and therefore an associated high risk of exposure for groups vulnerable to severe COVID-19.
A predictable pattern of COVID-19 seasonality has not yet been established. Nevertheless, time series of severe COVID-19 outcomes (hospital, ICU admissions COVID-19 deaths) since the beginning of the pandemic show that the impact of the disease has been much higher during the period corresponding to the traditional influenza season.
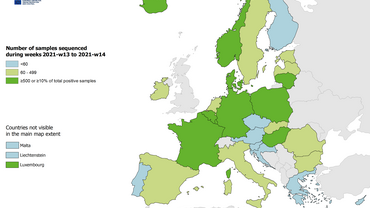
Omicron SARS-CoV-2 virus subvariants continue to dominate the SARS-CoV-2 virological landscape in the EU/EEA and globally. In the EU/EEA, several variants under investigation (VUI) including XBB.1.5, other XBB lineages and CH.1.1, have been increasing in proportion and XBB.1.5 became the dominant lineage by March 2023, without causing a deterioration in the epidemiological situation.
Since September 2022, bivalent vaccines targeting the Omicron sub-lineages BA.1 and BA.4/BA.5 have represented approximately 94% of the total vaccine doses administered, according to data reported in the EU/EEA (18 countries reporting).
Data currently available on vaccine effectiveness (VE) of monovalent and bivalent booster doses indicate added protection against severe outcomes in previously vaccinated individuals. In most cases, studies of the bivalent BA.4/5 mRNA COVID-19 vaccines were conducted during a time when Omicron BA4/5 or sub lineages of the Omicron variants were the dominant strains. For effectiveness of bivalent vaccines, longer follow-up is needed to determine the long-term protective effect of a bivalent booster against severe outcomes.
Evidence suggests that hybrid immunity confers strong protection against severe COVID-19, with high levels of protection lasting possibly beyond 12 months. However, it is likely that hybrid immunity has not developed uniformly across populations, with the elderly reportedly having the lowest rates.
Mathematical modelling has been undertaken at ECDC, based on the observed epidemiology of COVID-19 in EU/EEA countries, observed vaccine uptake of boosters in EU/EEA countries, review of the literature on vaccine effectiveness, waning and hybrid immunity. Modelling scenarios of campaigns restricted to once/twice a year and with modelling restricted to the population aged 50 years and above and 80 years and above, respectively, in the main analysis indicates as follows:
- An autumn 2023 vaccination campaign with an optimistic scenario of high vaccine uptake among individuals aged 60 years and above as a target group is expected to prevent an estimated 21−32% of the cumulative total all-age COVID-19-related hospitalisations across EU/EEA countries until 28 February 2024. The incremental gains in prevention are larger when targeting individuals aged 60 years and above instead of 80 years and above. The gains in prevention are similar, irrespective of whether individuals aged 50 years and above or 60 years and above are targeted.
- Combining an autumn 2023 vaccination campaign targeting individuals aged 60 years and above with a spring 2023 vaccination campaign targeting individuals aged 80 years and above can result in a substantial increase in the impact of vaccination (an estimated 36−44% reduction in hospitalisations), but only if the vaccine uptake is high in both the autumn and spring campaigns. A low vaccine uptake in the spring 2023 campaign followed by a high vaccine uptake in the autumn 2023 campaign in the same age groups (80 and 60 years, respectively) is only marginally different to an autumn 2023 campaign alone. This indicates that for the spring campaign to be effective at population level it is important to achieve a high vaccine uptake.
- Similar results were observed for prevented mortality and disability-adjusted life years (DALYs).
- When contrasting the overall impact with the efficiency of the different vaccination campaign scenarios, the per-dose effect increases with age for the target population. However, no substantial difference in efficiency is observed when comparing autumn and spring campaigns.
At present, four EU/EEA countries have published their approach/recommendations to COVID-19 vaccination campaigns for 2023. In four countries, spring vaccination campaigns are recommended, targeting vulnerable groups (individuals aged over 75 years, those who are immunocompromised and residents of long-term care facilities). For the autumn vaccination, two countries have announced campaigns targeting vulnerable groups, such as individuals aged 65 years and above, and individuals with underlying comorbidities.
Based on the elements summarised above, to decrease the impact of COVID-19, and the related hospitalisations and mortality expected during 2023, countries should plan for a continued roll-out of COVID-19 vaccines, particularly during the autumn/winter season, and take into account the following considerations:
- vaccination efforts should focus on protecting those aged over 60 years and other vulnerable individuals irrespective of age (such as those with underlying comorbidities and the immunocompromised) during the autumn/winter seasons 2023;
- to maximise individual protection, the offer of COVID-19 vaccination during spring 2023 to individuals aged over 80 years and to other vulnerable adults, irrespective of age, should also be considered. This could also have a substantial effect at population level, if the uptake is projected to be high;
- for the autumn/winter vaccination campaigns, countries should consider combined vaccination campaigns against COVID-19 and influenza, since this approach could be more efficient in terms of administration, logistics and costs.
- If a spring COVID-19 vaccination campaign is undertaken, there should be adequate time allowed between the spring and autumn campaigns.
- The above considerations are consistent with the recent highlights presented by WHO’s Strategic Advisory Group of Experts on Immunization (SAGE), which has defined high-, medium- and low-priority groups for continued COVID-19 vaccination with respect to the current epidemiological scenario. In its updated roadmap highlights, SAGE recommends an additional booster dose for the high-priority groups, either six or 12 months after the last dose, with the timeframe depending on factors such as age and immunocompromising condition. SAGE indicates that these recommendations should not be seen as continuous annual COVID-19 vaccine boosters.
- Overall, the decisions at country level related to COVID-19 vaccination for 2023 will continue to depend on a number of key evolving factors, such as the specific national epidemiological situation, possible virus evolution, availability of vaccines (including updated vaccines), vaccine effectiveness and protection over time, evidence on the effect of repeated boosters, degree of hybrid immunity across the population, projected vaccine uptake in different age groups, vaccine acceptance and the capacity of health systems to deliver vaccinations in the context of other competing public health priorities during the post-pandemic phase.
- Promoting acceptance and uptake of COVID-19 vaccination becomes challenging in the context of diminishing population interest in getting vaccinated and a perception of ‘return to normality’. Factors leading to declining uptake need to be identified, even in populations previously willing to be vaccinated. Future vaccination campaigns may consider developing targeted communication, focusing efforts on reaching high-priority groups through trusted channels and messengers, and providing clear information on which groups vaccination is being recommended to, the type of vaccines available and the timing. People should also be reminded why it is important to stay up-to-date with vaccination (particularly those in risk groups for severe COVID-19).