Monkeypox multi-country outbreak - second update
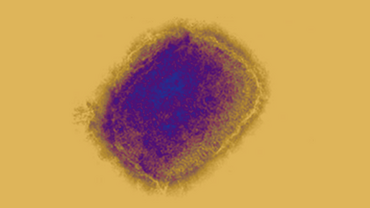
Since early May, and as of 11 October 2022, 20 455 confirmed cases of monkeypox (MPX) have been reported from 29 European Union/European Economic Area (EU/EEA) countries, including four deaths. As of 30 September, MPX confirmed cases reported from EU/EEA countries represented almost one third (29.7%) of the cases reported to the World Health Organization (WHO) globally (68 267 cases).
Executive summary
The weekly number of MPX cases reported in the EU/EEA peaked in July 2022 and a steady declining trend has been observed since, with only a few cases being reported at the time of this update. Multiple factors have probably contributed to the decline of this outbreak, including efforts in risk communication and community engagement, increasing immunity in the most affected population due to natural immunity and vaccination, and a decrease after the summer in large cultural and social events frequented by the main risk groups for this outbreak.
The majority of cases continue to be detected in males between 18 and 50 years (87%), and primarily among men who have sex with men (MSM). Summer mass gatherings and specific sexual practices have facilitated the transmission of MPX among MSM groups until now. Sporadic cases in women and children have also been reported. Cases in the current outbreak continue to present with a spectrum of symptoms and signs that differs from what has been described in past outbreaks of MPX in endemic countries. In general, cases have presented in this outbreak with relatively mild symptoms although some patients describe significant discomfort, pain and complications. From the total number of cases reported in the EU/EEA, 1.1% have required hospitalisation for clinical care and five cases were admitted to intensive care.
Based on evidence in the current outbreak and the declining number of new infections, the overall risk of MPX infection is assessed as moderate for MSM and low for the broader population.
Early diagnosis, isolation, and effective contact tracing, supported by appropriate vaccination strategies remain key for the effective control of this outbreak. Mass vaccination against MPX is currently not required nor recommended. Considering limitations in vaccine supplies, primary preventive vaccination (PPV) and post-exposure preventive vaccination (PEPV) strategies may be combined focusing on individuals at substantially higher risk of exposure and close contacts of cases, respectively. PPV strategies should prioritise gay, bisexual, or other men or transgender people who have sex with men who are at higher risk of exposure based on epidemiological or behavioural criteria. Individuals at risk for occupational exposure should be considered based on risk assessment. Vaccination strategies will need to be kept under review as evidence on effectiveness is accumulated and adapted to the situation in each country according to the trajectory of the outbreak.
While some encouraging preliminary evidence is emerging on the performance of the MVA-BN vaccine, more robust data on vaccine efficacy and effectiveness is needed. Targeted national vaccination programmes should be implemented within a framework of collaborative research and clinical trial protocols with standardised data collection tools for clinical and outcome data. Health promotion interventions and community engagement are also critical to ensure effective outreach and high vaccine acceptance and uptake among those most at risk of exposure.
Despite the improving epidemiological situation, it is important to continue active risk communication and community engagement efforts with the affected population to prevent a resurgence. Activities to increase awareness of health professionals across specialties should also continue in order to ensure prompt diagnosis and the appropriate management of cases and contacts. Testing services for orthopoxvirus should be available, while support to sexual health services is important to the continuation of case detection, contact tracing, and management of cases.
Future considerations for the evolution of the MPX outbreak and for preventing similar outbreaks are outlined, including the scenario that the outbreak resurges, it causes a continued low number of new cases almost exclusively among MSM, which is considered more likely currently, MPX wanes and finally it is eliminated in EU/EEA countries through concerted efforts in the European region.
What’s new in this update
This update was triggered by the continuous decline of case numbers since the end of July 2022. It includes an updated risk assessment for the most affected sub-population and health professionals based on evidence from this outbreak and new information on MPX vaccine effectiveness. It reinforces the need for continued investment in the response to the MPX outbreak and finally, it includes a section on considerations for the evolution of the outbreak and for preventing similar outbreaks with qualitative scenarios.
Download