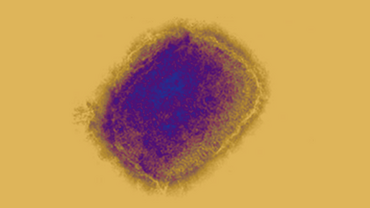
Public health considerations for mpox in EU/EEA countries
Since 16 May 2022, and as of 4 April 2023, 21 170 cases of mpox (formerly known as monkeypox) have been reported by countries within the European Union/European Economic Area (EU/EEA).
Executive summary
Early diagnosis, isolation, partner notification, and contact tracing, supported by appropriate vaccination strategies and behaviour change in case of increased transmission, remain key for the effective control of this outbreak. From the beginning of the current multi-country outbreak, vaccination has been considered as an additional measure to complement primary public health interventions. Mass vaccination against mpox was not required nor recommended and such approach remains valid today. Mpox vaccines can be used as post-exposure vaccination (PEPV) or as primary preventive (pre-exposure) vaccination (PPV). Vaccination programmes must be backed by thorough surveillance and contact tracing and accompanied by a strong information campaign and robust pharmacovigilance.
The number of countries rolling out mpox vaccination campaigns has increased since the beginning of the outbreak. Based on the data reported in relation to the administration of vaccine doses, the vaccine strategies adopted focused on PPV, targeting males aged between 25 and 59 years, and subcutaneous administration. Between September 2022 and February 2023, a total of 336 976 vaccine doses were administered in 25 EU/EEA countries. PEPV was implemented in the early months of the outbreak, but it was quickly followed by PPV, with the majority of doses (86%) administered as PPV for the overall period. An observed increasing trend in the proportion of ‘second doses’ of the total number of doses administered monthly reported over time suggests that countries are completing the standard primary vaccination schedule (two doses), while the proportion of ‘first doses’ (new vaccinees) is decreasing.
While some encouraging preliminary evidence is emerging on the performance of the MVA-BN vaccine, more robust data on vaccine efficacy and effectiveness are needed. It is important that if targeted national vaccination programmes are considered, they should be optimally implemented within a framework of collaborative research and clinical trial protocols with standardised data collection tools. Health promotion interventions and community engagement are also critical to ensure effective outreach and high vaccine acceptance and uptake among those most at risk of exposure.
Risk communication and community engagement are also essential to achieving results across all the proposed measures: testing, partner notification or contact tracing, isolation of cases, vaccination, and behaviour change. Close collaboration with civil society and community-based organisations serving populations at risk is key for the success of risk communication and community engagement efforts. This also includes liaising with venue owners and organisers of Pride events. Testing should be made available to improve rapid access, particularly in clinicalsettings that serve gay, bisexual or other men or transgender people who have sex with men, as this is where the populations at highest risk are likely to access care. There is a need to raise awareness among clinicians that new cases of mpox may arise in the spring and summer. Clinicians should be made aware of how to rapidly detect and report cases of mpox to public health authorities to enable timely and responsive public health interventions.
Download