Spread of hepatitis A virus strains of genotype IB in several EU countries and the United Kingdom
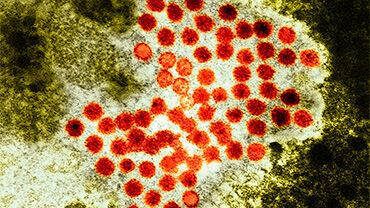
Clusters and outbreaks of hepatitis A virus (HAV) genotype IB with four unique but closely related HAV sequences have been reported in six European Union (EU) countries and in the United Kingdom (UK).
As of 29 September 2022, 303 cases with identical or closely related HAV strains have been identified in Austria (7), Germany (8), Hungary (161), the Netherlands (8), Slovenia (35), Sweden (8), and the UK (76). Currently available epidemiological and microbiological data suggest that human-to-human transmission has occurred, and possibly also transmission through contaminated food.
On 15 February 2022, Hungary reported an outbreak of HAV genotype IB with the disease onset of the first case in early December 2021. To date, 161 cases (139 males, 22 females) have been confirmed with this strain in the National Hepatitis Reference Laboratory in Hungary. The weekly number of reported hepatitis A cases have been declining since June 2022. Several infected people identified themselves as men who have sex with men (MSM), suggesting possible transmission among sexual contacts. Several patients have been hospitalised.
In July 2022, a foodborne outbreak was suspected with a link to a restaurant in Hungary, where 16 people fell ill with HAV IB infection. Some of the patients reported consuming cold soup made with frozen berries. In the UK, no clear source of infection has been identified, but epidemiological investigations so far indicate possible foodborne infections in addition to person-to-person transmission. Germany, the Netherlands, and Sweden have reported a total of nine cases infected with strains matching the sequences of the UK strain. Investigations of these cases didn’t find any clear risk factors for infection such as a travel history or consumption of berries. Further investigations are ongoing.
HAV is highly transmissible through contaminated water, food, and via the faecal–oral route among close contacts (e.g. household contacts, sexual contacts, and contacts in day-care centres or schools), with an average incubation period of four weeks, ranging from two to six weeks. The virus is highly resistant to environmental conditions as well as to several preservation methods like acidification or freezing. Therefore, possible food-borne transmission should be investigated when several cases are reported within a short period.
Practising good hand hygiene – including thoroughly washing hands with soap after using the bathroom, changing nappies, and before preparing or eating food – plays an important role in preventing the spread of hepatitis A. Scaling up surveillance to detect and investigate sporadic and clusters of cases possibly associated with foodborne transmission in collaboration with food safety authorities is essential.
MSM are at risk of HAV infection when engaging in sexual practices that facilitate faecal-oral transmission of the virus. Hepatitis A vaccination, which is safe and highly effective, is the main option for response in the context of the current circulation of HAV genotype IB among MSM. The World Health Organisation and most EU/EEA countries recommend hepatitis A vaccination for MSM.
Besides vaccination, other options can contribute to the prevention of transmission among MSM: the use of condoms for anal sex, which have the additional benefit of offering protection against other sexually transmitted infections and good personal hygiene (e.g. washing hands and genital areas before and after sex). For the provision of primary prevention advice, authorities should consider engaging with civil society, social media, media outlets and dating apps to raise awareness among MSM about the risk of contracting HAV and the importance of vaccination. MSM who have already contracted the infection should be referred to sexual health services for further testing.