A systematic literature review of interventions to increase linkage to care and adherence to treatment for hepatitis B and C, HIV and tuberculosis among people who inject drugs
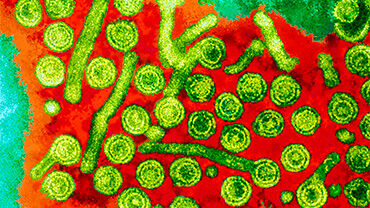
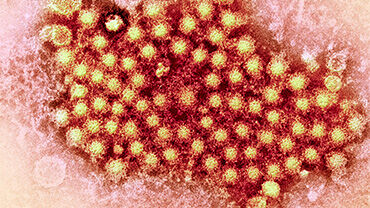
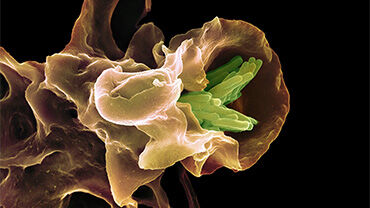
The purpose of this review was to identify and synthesise the existing evidence on effectiveness of interventions targeting people who inject drugs at two stages of the care cascade: linkage to care and adherence to treatment of HIV, hepatitis B/C and TB.
Executive summary
Background
This systematic literature review of interventions to increase linkage to care and adherence to treatment for hepatitis B and C, HIV and tuberculosis (TB) among people who inject drugs was conducted as part of the update process of the joint European Centre for Disease Prevention and Control (ECDC) and European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) guidance, ’Prevention and control of infectious diseases among people who inject drugs’ (published in 2011). The purpose of this review was to identify and synthesise the existing evidence on effectiveness of interventions targeting people who inject drugs at two stages of the care cascade: linkage to care and adherence to treatment of HIV, hepatitis B/C and TB.
Methods
The systematic review was conducted following Preferred Reporting Items for Systematic Reviews and Meta- Analyses (PRISMA) guidelines. A protocol was developed and published on PROSPERO together with the search strategy.
The primary research question regarding interventions that impact linkage to care and adherence to treatment of infections among people who inject drugs was formulated based on a PICO format and included the following elements:
- P (population): people who inject drugs or people receiving OST with chronic HBV, HCV, HIV infection and/or TB;
- I (intervention): any intervention to increase linkage to care or enhance adherence to treatment;
- C (comparator): people who inject drugs or OST comparator group with no intervention or receiving usual or routine care; and
- O (outcome): linkage to care: ‘visit’ and ‘treatment initiation’ (TI) and adherence to treatment: ‘sustained virological response’ (SVR12/SVR24), ‘treatment adherence’ (TA), ‘treatment completion’ (TC), or change to low viral load/undetectable ‘viral load’ (VL).
Barriers to linkage to care and adherence to treatment were collected as secondary outcomes from the eligible studies. Searches in five electronic databases covered the period from 1 January 2011 to 8 July 2020 with no language restrictions and included all the European Union (EU)/ European Economic Area (EEA)/European Free Trade Association (EFTA) countries, EU candidate countries, the United Kingdom, the United States, Canada, Australia, and New Zealand. Titles, abstracts, and full texts were reviewed for inclusion by two independent reviewers, with a third reviewer acting as an arbiter. Data were extracted using a pre-specified, previously piloted data extraction form. The study risk of bias was assessed using the Effective Public Health Practice Project (EPHPP) tool [1], while study quality was determined in accordance with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system described by Guyatt et al. (2008) [2].
A narrative synthesis of the findings was conducted of publications addressing the impact of interventions on linkage to care and adherence to treatment. The evidence base identified through this review was critically reviewed by a panel of experts appointed by ECDC and EMCDDA.
Results
This systematic literature review of interventions to increase linkage to care and adherence to treatment for infections among people who inject drugs retrieved 25 eligible studies that were included in the analysis. These studies represented a diverse group of interventions spanning various settings and focusing on one or two of the infections of interest. Most studies (20) focused on HCV, with only four studies on HIV and one on TB. There were no eligible studies reporting interventions for HBV. All included studies were conducted in high-income countries (the United States, Canada, Australia, New Zealand, Italy, Germany, Portugal, Austria, the United Kingdom, Spain, and one multicentre trial at sites in the United States and Europe).
For increasing linkage to HCV care, the results suggest that integrated care approaches, nurse case management, and peer involvement, as well as multidisciplinary services and cooperation between providers, especially when involving pharmacies and primary care settings, are promising strategies to facilitate treatment- seeking and improving access to care for people who inject drugs. For increasing linkage to HIV care, identified evidence was sparse and of very low quality. Regarding interventions to increase adherence to treatment, major differences were identified between the four infectious diseases due to a diversity of treatment options and durations. Adherence to HCV treatment was improved by peer mentoring, integrated care, and primary care approaches. For adherence to HIV treatment, only non-randomised and rather low-quality studies were identified, which resulted in a low certainty of evidence ratings. One study evaluated adherence to TB treatment through cooperation between services, but the unclear certainty of evidence due to low quality did not allow an interpretation of effectiveness.
Conclusions
This review, covering the period between 2011 and 2020, identified several interventions that can improve linkage to care and adherence to treatment of infections (in particular of HCV) among people who inject drugs and can inform public health decision-making and practice. It also highlights the paucity of well-designed randomised control trials (RCTs) or comparative studies evaluating interventions to enhance linkage to care and adherence to treatment, especially in relation to HBV, HIV and TB. There were no studies evaluating interventions to enhance linkage to HBV and TB care, and only one study assessing adherence to TB treatment. This review calls for well-designed studies evaluating interventions for an improved and simplified care cascade for infectious diseases among people who inject drugs. Outcomes of this systematic review provide a direction for policy-makers, public health researchers and national and international programme coordinators involved in the prevention and control of infectious disease among the people who inject drugs in EU/EEA countries and elsewhere.
Download